What is monkeypox?
Monkeypox is a rare disease caused by infection with the monkeypox virus. Monkeypox virus is part of the same family of viruses as variola virus, the virus that causes smallpox. Monkeypox symptoms are similar to smallpox symptoms, but milder, and monkeypox is rarely fatal. Monkeypox is not related to chickenpox.
Monkeypox was discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research. Despite being named “monkeypox,” the source of the disease remains unknown. However, African rodents and non-human primates (like monkeys) might harbor the virus and infect people.
The first human case of monkeypox was recorded in 1970. Prior to the 2022 outbreak, monkeypox had been reported in people in several central and western African countries. Previously, almost all monkeypox cases in people outside of Africa were linked to international travel to countries where the disease commonly occurs or through imported animals. These cases occurred on multiple continents.
What are the symptoms?
ruses as smallpox. Monkeypox symptoms are similar to smallpox symptoms, but milder; and monkeypox is rarely fatal. Monkeypox is not related to chickenpox.
Symptoms of monkeypox can include:
- Fever
- Headache
- Muscle aches and backache
- Swollen lymph nodes
- Chills
- Exhaustion
- A rash that can look like pimples or blisters that appears on the face, inside the mouth, and on other parts of the body, like the hands, feet, chest, genitals, or anus.
The rash goes through different stages before healing completely. The illness typically lasts 2-4 weeks. Sometimes, people get a rash first, followed by other symptoms. Others only experience a rash.
How can I get tested for monkeypox?
How is monkeypox spread?
Monkeypox spreads in different ways. The virus can spread from person-to-person through:
- direct contact with the infectious rash, scabs, or body fluids
- respiratory secretions during prolonged, face-to-face contact, or during intimate physical contact, such as kissing, cuddling, or sex
- touching items (such as clothing or linens) that previously touched the infectious rash or body fluids
- pregnant people can spread the virus to their fetus through the placenta
- It’s also possible for people to get monkeypox from infected animals, either by being scratched or bitten by the animal or by preparing or eating meat or using products from an infected animal.
Monkeypox can spread from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. The illness typically lasts 2-4 weeks. People who do not have monkeypox symptoms cannot spread the virus to others. At this time, it is not known if monkeypox can spread through semen or vaginal fluids.
How can you prevent monkeypox?
Take the following steps to prevent getting monkeypox:
- Avoid close, skin-to-skin contact with people who have a rash that looks like monkeypox.
- Do not touch the rash or scabs of a person with monkeypox.
- Do not kiss, hug, cuddle or have sex with someone with monkeypox.
- Do not share eating utensils or cups with a person with monkeypox.
- Do not handle or touch the bedding, towels, or clothing of a person with monkeypox.
- Wash your hands often with soap and water or use an alcohol-based hand sanitizer.
- In Central and West Africa, avoid contact with animals that can spread monkeypox virus, usually rodents and primates. Also, avoid sick or dead animals, as well as bedding or other materials they have touched.
If you are sick with monkeypox
- Isolate at home
- If you have an active rash or other symptoms, stay in a separate room or area away from people or pets you live with, when possible.
Vaccination Information
Vaccine supply is limited. We have received a limited number of doses from the federal government, and we are making it available as quickly as possible.
Current Vaccine Criteria
- Known contacts who are identified by public health via case investigation, contact tracing, and risk exposure assessments
- Are you a person of any gender identity or sexual orientation with any of the following:
- Have had multiple or anonymous sex partners with men who have sex with men in the last 14 days
- Have had skin-to-skin or intimate contact (e.g., kissing, hugging) with persons who have had a rash or are suspected of having monkeypox in the last 14 days.
- Have had skin-to-skin or intimate contact (e.g., kissing, hugging) with persons at large venues or events in the past 14 days.
- Have engaged in commercial and/or transactional sex in the past 14 days (e.g., sex in exchange for money, shelter, food, and other goods or needs)
- Are HIV positive, or on HIV PrEP, or diagnosed with a sexually transmitted infection (STI) in the last 90 days.
- You do not have any symptoms of monkeypox and you have not been diagnosed with a monkeypox infection since May 17, 2022.
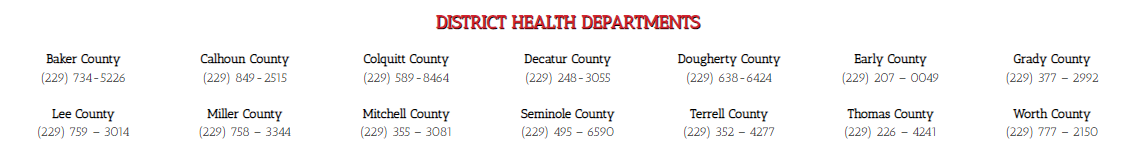
If you meet the current criteria for the monkeypox vaccine, you can register online at: https://gta-vras.powerappsportals.us/en-US/ or call your local health department.
When properly administered before or after a recent exposure, vaccines can be effective tools at protecting people against monkeypox illness. The following vaccination strategies are being used in the United States:
Monkeypox Vaccine Post-Exposure Prophylaxis (PEP)
- For the current outbreak, this approach can be considered as “standard PEP” for monkeypox. People can be vaccinated following exposure to monkeypox to help prevent illness from monkeypox virus. It is important that states and other jurisdictions identify contacts of confirmed or probable monkeypox cases to offer vaccine for PEP and to monitor for any early signs of illness.
- CDC recommends that the vaccine be given within 4 days from the date of exposure for the best chance to prevent onset of the disease.
- If given between 4 and 14 days after the date of exposure, vaccination may reduce the symptoms of disease, but may not prevent the disease. However, when coupled with self-isolation and other prevention measures when symptoms first occur, PEP is important for controlling outbreaks and preventing further transmission of monkeypox.
Outbreak Response Monkeypox Vaccine Post-Exposure Prophylaxis (PEP)++
- For the current outbreak, this expanded approach can be considered as “individual-directed PEP” for monkeypox; public health officials refer to it as “expanded PEP” or “PEP plus-plus” or “PEP++”.
- People with certain risk factors are more likely to have been recently exposed to monkeypox. The PEP++ approach aims to reach these people for post-exposure prophylaxis, even if they have not had documented exposure to someone with confirmed monkeypox.
- When coupled with self-isolation and other prevention measures when symptoms first occur, PEP++ may help slow the spread of the disease in areas with large numbers of monkeypox cases—which would suggest a higher level of monkeypox virus transmission.
Monkeypox Vaccine Pre-Exposure Prophylaxis (PrEP)
- This approach refers to administering vaccine to someone at high risk for monkeypox (for example, laboratory workers who handle specimens that might contain monkeypox virus).
- At this time, most clinicians in the United States and laboratorians not performing the orthopoxvirus generic test to diagnose orthopoxviruses, including monkeypox virus, are not advised to receive monkeypox vaccine PrEP.
Need More Information?
- Please visit the Centers for Disease Control and Prevention: https://www.cdc.gov/poxvirus/monkeypox/index.html
- Contact your Local County Health Department
